Understanding Bone Loss in the Jaw: Causes, Consequences, and Solutions
Jawbone resorption, or bone loss, occurs when the jawbone deteriorates, impacting chewing, speaking, and facial appearance. This common condition affects millions globally and doesn’t regenerate naturally without treatment. Recognizing its causes, warning signs, and treatment options is essential to maintaining oral health and preventing serious complications.
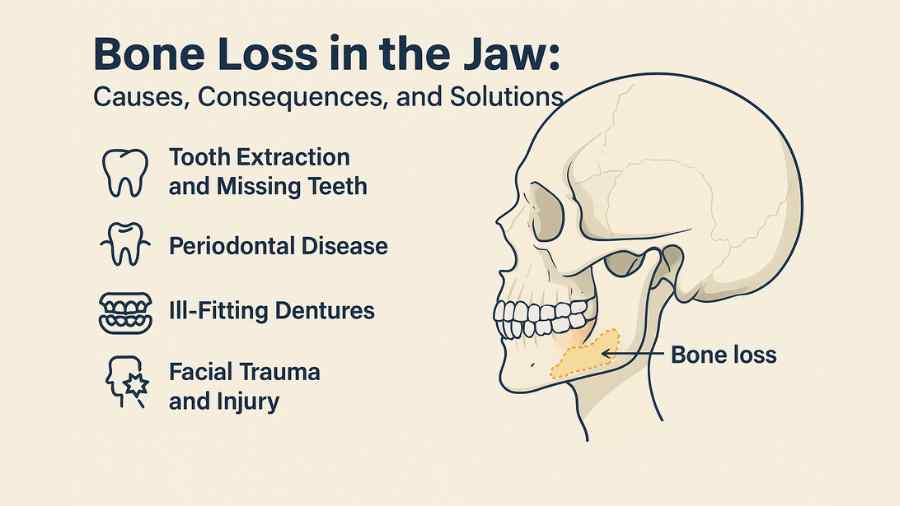
What Causes Bone Loss in the Jaw?
Several factors can trigger jawbone deterioration, with some causes being more preventable than others. Understanding these root causes helps patients and dental professionals develop targeted treatment strategies.
Tooth Extraction and Missing Teeth
When you lose a tooth—whether due to extraction, injury, or natural causes—the surrounding jawbone begins to deteriorate almost immediately. Your teeth provide constant stimulation to the jawbone through everyday activities like chewing and biting. Without this stimulation, the bone tissue starts to resorb, or break down.
Research shows that patients can lose up to 25% of their jawbone width within the first year after tooth extraction. This process accelerates over time, with continued bone loss occurring for years following tooth removal.
Periodontal Disease
Gum disease represents one of the most significant threats to jawbone health. When bacteria accumulate below the gum line, they release toxins that trigger an inflammatory response. Over time, this chronic inflammation destroys the tissues and bone that support your teeth.
Advanced periodontal disease can cause extensive bone loss, leading to tooth mobility and eventual tooth loss if left untreated. The progression from gingivitis to advanced periodontitis can occur gradually, making regular dental monitoring essential.
Ill-Fitting Dentures
Traditional dentures rest on top of the gums rather than stimulating the underlying jawbone. While they may restore some chewing function, they don’t provide the mechanical stimulation necessary to maintain bone density.
Poorly fitted dentures can accelerate bone loss by creating uneven pressure points and friction against the gums. Over time, this leads to further bone resorption and the need for denture adjustments or replacements.
Facial Trauma and Injury
Accidents, sports injuries, and other facial trauma can damage jawbone tissue directly. Even when teeth remain intact after an injury, the surrounding bone may be compromised, leading to gradual deterioration over time.
Some injuries may not show immediate signs of bone damage, making follow-up care and monitoring crucial for detecting delayed complications.
Medical Conditions and Medications
Certain medical conditions, including osteoporosis, diabetes, and autoimmune disorders, can increase your risk of jawbone loss. Additionally, some medications—particularly bisphosphonates used to treat osteoporosis—can affect jawbone health and healing.
Radiation therapy to the head and neck region can also damage jawbone tissue, creating long-term complications for patients undergoing cancer treatment.
Consequences of Untreated Bone Loss
Ignoring jawbone deterioration can lead to progressively worsening complications that affect both your appearance and function.
Facial Structure Changes
As jawbone tissue diminishes, your facial structure begins to change dramatically. The lower third of your face may appear shorter, creating a collapsed or sunken appearance. Your lips may lose support, leading to increased wrinkling around the mouth.
These changes can add years to your appearance and significantly impact self-confidence. The progression typically accelerates over time, making early intervention crucial for preserving your natural facial contours.
Compromised Oral Function
Bone loss directly affects your ability to chew food effectively and speak clearly. As the jawbone shrinks, remaining teeth may become loose or shift position, creating bite problems and making it difficult to eat certain foods.
Speech patterns may change as well, particularly affecting sounds that require precise tongue placement against the teeth. These functional changes can impact nutrition, social interactions, and overall quality of life.
Limited Treatment Options
Advanced bone loss can severely limit your future treatment options. Dental procedures that require adequate bone support—such as dental implant placement—may become impossible without extensive bone grafting procedures.
The longer bone loss continues untreated, the more complex and expensive future treatments become. Early intervention provides the best outcomes and preserves the most treatment options.
Treatment Options for Jawbone Loss
Modern dentistry offers several effective approaches for addressing bone loss and restoring jawbone health.
Bone Grafting Procedures
Bone grafting represents the gold standard for rebuilding lost jawbone tissue. During this procedure, your dentist or oral surgeon places grafting material—which may come from your own body, a donor source, or synthetic materials—into areas where bone loss has occurred.
The grafting material serves as a scaffold, encouraging your body to grow new bone tissue. Over several months, the graft material integrates with your existing bone, creating a strong foundation for future dental work.
Different types of bone grafts include autografts (from your own body), allografts (from human donors), xenografts (from animal sources), and alloplasts (synthetic materials). Your dental professional will recommend the most appropriate option based on your specific needs.
Dental Implant Placement
Dental implants provide the most effective long-term solution for preventing continued bone loss. These titanium posts are surgically placed into the jawbone, where they fuse with the surrounding tissue through a process called osseointegration.
Once integrated, dental implants function like natural tooth roots, providing the mechanical stimulation necessary to maintain bone density. A dental implant marketing company might emphasize these benefits when educating patients about treatment options, but the scientific evidence supporting implant therapy speaks for itself.
Studies show that dental implants can halt bone loss and even promote new bone formation in treated areas. This makes them superior to traditional dentures or bridges for long-term oral health maintenance.
Sinus Lift Procedures
For patients with bone loss in the upper jaw, sinus lift procedures can create additional space for bone grafting and implant placement. During this surgery, the sinus membrane is gently lifted, and bone grafting material is placed in the newly created space.
This technique allows for successful implant placement even in cases where significant bone loss has occurred in the posterior upper jaw.
Prevention Strategies
Preventing bone loss is always preferable to treating it after it occurs. Several proactive strategies can help maintain optimal jawbone health throughout your lifetime.
Maintain Excellent Oral Hygiene
Consistent brushing, flossing, and antimicrobial rinse use help prevent periodontal disease—one of the leading causes of jawbone loss. Focus on thorough plaque removal along the gum line, where bacteria tend to accumulate.
Consider using an electric toothbrush, which research shows may be more effective at removing plaque than manual brushing. Water flossers can also help clean areas that traditional floss might miss.
Schedule Regular Dental Check-ups
Professional cleanings and examinations allow your dental team to detect early signs of gum disease and other conditions that could lead to bone loss. Most patients benefit from visits every six months, though some may require more frequent monitoring.
During these visits, your dentist can perform periodontal probing to measure gum pocket depths and take X-rays to monitor bone levels over time.
Address Tooth Loss Promptly
If you lose a tooth, discuss replacement options with your dentist as soon as possible. The earlier you address tooth loss, the more bone structure you can preserve for future treatments.
Even if you’re not ready for immediate implant placement, your dentist may recommend socket preservation techniques to minimize bone loss following extraction.
Manage Risk Factors
Work with your healthcare providers to manage medical conditions that could affect bone health. This might include optimizing diabetes control, addressing nutritional deficiencies, or modifying medications when possible.
If you participate in contact sports or other high-risk activities, consider wearing a custom-fitted mouthguard to protect against facial trauma.
Conclusion
Now that you understand the importance of preserving bone after a tooth extraction, it’s important to work closely with your dentist or oral surgeon to choose the best method for you.



